“Despite the projected growth in market applications and abundant investment capital, there is a danger that legal and ethical concerns related to genetic research could put the brakes on gene editing technologies and product programs emanating therefrom.”
As society adjusts to a new world of social distance and remote everything, rapid advancements in the digital, physical, and biological spheres are accelerating fundamental changes to the way we live, work, and relate to one another. What Klaus Schwab prophesized in his 2015 book, The Fourth Industrial Revolution, is playing out before our very eyes. Quantum computing power, a network architecture that is moving function closer to the edge of our interconnected devices, bandwidth speeds of 5G and beyond, natural language processing, artificial intelligence, and machine learning are all working together to accelerate innovation in fundamental ways. Given the global pandemic, in the biological sphere, government industrial policy drives the public sector to work hand-in-glove with private industry and academia to develop new therapies and vaccines to treat and prevent COVID-19 and other lethal diseases. This post will envision the future of gene editing technologies and the legal and ethical challenges that could imperil their mission of saving lives.
What is Genome Editing?
There are thousands of diseases occurring in humans, animals, and plants caused by aberrant DNA sequences. Traditional small molecule and biologic therapies have only had minimal success in treating many of these diseases because they mitigate symptoms while failing to address the underlying genetic causes. While human understanding of genetic diseases has increased tremendously since the mapping of the human genome in the late 1990s, our ability to treat them effectively has been limited by our historical inability to alter genetic sequences.
The science of gene editing was born in the 1990s, as scientists developed tools such as zinc-finger nucleases (ZFNs) and TALE nucleases (TALENs) to study the genome and attempt to alter sequences that caused disease. While these systems were an essential first step to demonstrate the potential of gene editing, their development was challenging in practice due to the complexity of engineering protein-DNA interactions.
Then, in 2011, Dr. Emmanuelle Charpentier, a French professor of microbiology, genetics, and biochemistry, and Jennifer Doudna, an American professor of biochemistry, pioneered a revolutionary new gene-editing technology called CRISPR/Cas9. Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR) and Cas9 stands for CRISPR-associated protein 9. In 2020, the revolutionary work of Drs. Charpentier and Doudna developing CRISPR/Cas9 were recognized with the Nobel Prize for Chemistry. The technology was also the source of a long-running and high-profile patent battle between two groups of scientsists.
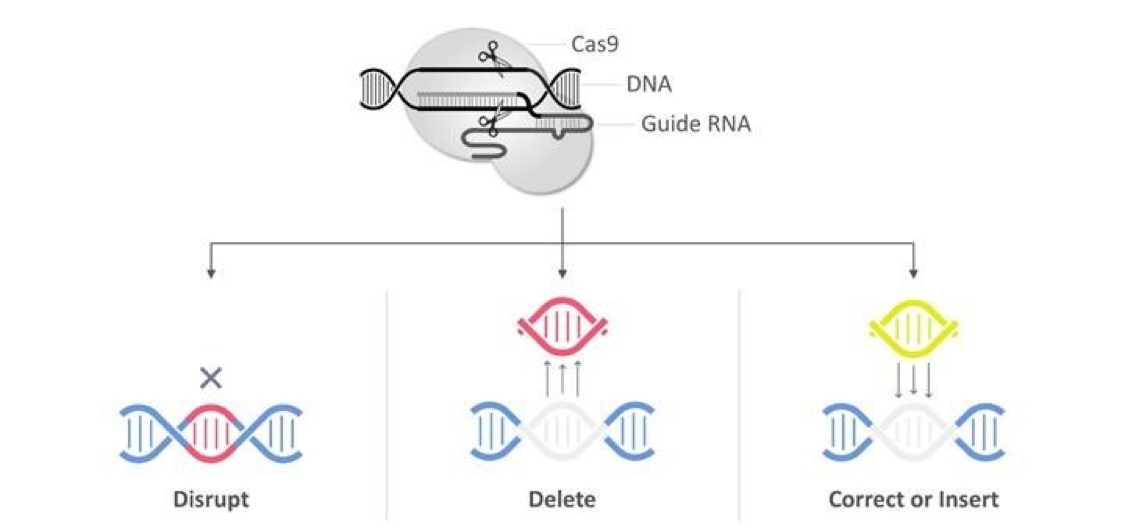
CRISPR/Cas9 for gene editing came about from a naturally occurring viral defense mechanism in bacteria. The system is cheaper and easier to use than previous technologies. It delivers the Cas9 nuclease complexed with a synthetic guide RNA (gRNA) into a cell, cutting the ’cell’s genome at the desired location, allowing existing genes to be removed and new ones added to a living organism’s genome. The technique is essential in biotechnology and medicine as it provides for the genomes to be edited in vivo with extremely high precision, efficiently, and with comparative ease. It can create new drugs, agricultural products, and genetically modified organisms or control pathogens and pests. More possibilities include the treatment of inherited genetic diseases and diseases arising from somatic mutations such as cancer. However, its use in human germline genetic modification is highly controversial.
The following diagram from CRISPR Therapeutics AG, a Swiss company, illustrates how it functions:
 Market Applications
Market Applications
In the 1990s, nanotechnology and gene editing were necessary plot points for science fiction films. In 2020, developments like nano-sensors and CRISPR gene editing technology have moved these technologies directly into the mainstream, opening a new frontier of novel market applications. According to The Business Research Company, the global CRISPR technology market reached a value of nearly $700 million in 2019, is expected to more than double in 2020, and reach $6.7 billion by 2030. Market applications target all forms of life, from animals to plants to humans.
Gene editing’s primary market applications are for the treatment of genetically-defined diseases. CRISPR/Cas9 gene editing promises to enable the engineering of genomes of cell-based therapies and make them safer and available to a broader group of patients. Cell therapies have already begun to make a meaningful impact on specific diseases, and gene editing helps to accelerate that progress across diverse disease areas, including oncology and diabetes.
In the area of human therapy, millions of people worldwide suffer from genetic conditions. Gene-editing technologies like CRISPR-Cas9 have introduced a way to address the cause of debilitating illnesses like cystic fibrosis and create better interventions and therapies. They also have promising market applications for agriculture, food safety, supply, and distribution. For example, grocery retailers are even looking at how gene editing could impact the products they sell. Scientists have created gene-edited crops like non-browning mushrooms and mildew-resistant grapes – experiments that are part of an effort to prevent spoilage, which could ultimately change the way food is sold.
Investment Capital
Despite the inability to travel and conduct face-to-face meetings, attend industry conferences or conduct business other than remotely or with social distance, the investment markets for venture, growth, and private equity capital, as well as corporate R&D budgets, have remained buoyant through 2020 to date. Indeed, the third quarter of 2020 was the second strongest quarter ever for VC-backed companies, with 88 companies raising rounds worth $100 million or more according to the latest PwC/Moneytree report. Healthcare startups raised over $8 billion in the quarter in the United States alone. Gene-editing company Mammouth Biosciences raised a $45 million round of Series B capital in the second quarter of 2020. CRISPR Therapeutics AG raised more in the public markets in primary and secondary capital.
Bayer, Humboldt Fund and Leaps are co-leading a $65 million Series A round for Metagenomi, a biotech startup launched by UC Berkeley scientists. Metagenomi, which will be run by Berkeley’s Brian Thomas, is developing a toolbox of CRISPR- and non-CRISPR-based gene-editing systems beyond the Cas9 protein. The goal is to apply machine learning to search through the genomes of these microorganisms, finding new nucleases that can be used in gene therapies. Other investors in the Series A include Sozo Ventures, Agent Capital, InCube Ventures and HOF Capital. Given the focus on new therapies and vaccines to treat the novel coronavirus, we expect continued wind in the sails for gene-editing companies, particularly those with strong product portfolios that leverage the technology.
Legal and Ethical Considerations
Despite the projected growth in market applications and abundant investment capital, there is a danger that legal and ethical concerns related to genetic research could put the brakes on gene-editing technologies and product programs emanating therefrom. The possibility of off-target effects, lack of informed consent for germline therapy, and other ethical concerns could cause government regulators to put a stop on important research and development required to cure disease and regenerate human health.
Gene-editing companies can only make money by developing products that involve editing the human genome. The clinical and commercial success of these product candidates depends on public acceptance of gene-editing therapies for the treatment of human diseases. Public attitudes could be influenced by claims that gene editing is unsafe, unethical, or immoral. Consequently, products created through gene editing may not gain the acceptance of the government, the public, or the medical community. Adverse public reaction to gene therapy, in general, could result in greater government regulation and stricter labeling requirements of gene-editing products. Stakeholders in government, third-party payors, the medical community, and private industry must work to create standards that are both safe and comply with prevailing ethical norms.
The most significant danger to growth in gene-editing technologies lies in ethical concerns about their application to human embryos or the human germline. In 2016, a group of scientists edited the genome of human embryos to modify the gene for hemoglobin beta, the gene in which a mutation occurs in patients with the inherited blood disorder beta thalassemia. Although conducted in non-viable embryos, it shocked the public that scientists could be experimenting with human eggs, sperm, and embryos to alter human life at creation. Then, in 2018, a biophysics researcher in China created the first human genetically edited babies, twin girls, causing public outcry (and triggering government sanctioning of the researcher). In response, the World Health Organization established a committee to advise on the creation of standards for gene editing oversight and governance standards on a global basis.
Some influential non-governmental agencies have called for a moratorium on gene editing, particularly as applied to altering the creation or editing of human life. Other have set forth guidelines on how to use gene-editing technologies in therapeutic applications. In the United States, the National Institute of Health has stated that it will not fund gene-editing studies in human embryos. A U.S. statute called “The Dickey-Wicker Amendment” prohibits the use of federal funds for research projects that would create or destroy human life. Laws in the United Kingdom prohibit genetically modified embryos from being implanted into women. Still, embryos can be altered in research labs under license from the Human Fertilisation and Embryology Authority.
Regulations must keep pace with the change that CRISPR-Cas9 has brought to research labs worldwide. Developing international guidelines could be a step towards establishing cohesive national frameworks. The U.S. National Academy of Sciences recommended seven principles for the governance of human genome editing, including promoting well-being, transparency, due care, responsible science, respect for persons, fairness, and transnational co-operation. In the United Kingdom, a non-governmental organization formed in 1991 called The Nuffield Council has proposed two principles for the ethical acceptability of genome editing in the context of reproduction. First, the intervention intends to secure the welfare of the individual born due to such technology. Second, social justice and solidarity principles are upheld, and the intervention should not result in an intensifying of social divides or marginalizing of disadvantaged groups in society. In 2016, in application of the same, the Crick Institute in London was approved to use CRISPR-Cas9 in human embryos to study early development. In response to a cacophony of conflicting national frameworks, the International Summit on Human Gene Editing was formed in 2015 by NGOs in the United States, the United Kingdom and China, and is working to harmonize regulations global from both the ethical and safety perspectives. As CRISPR co-inventor Jennifer Doudna has written in a now infamous editorial in SCIENCE, “stakeholders must engage in thoughtfully crafting regulations of the technology without stifling it.”
Where Do We Go from Here?
The COVID-19 pandemic has forced us to rely more on new technologies to keep us healthy, adapt to working from home, and more. The pandemic makes us more reliant on innovative digital, biological, and physical solutions. It has created a united sense of urgency among the public and private industry (together with government and academia) to be more creative about using technology to regenerate health. With continued advances in computing power, network architecture, communications bandwidths, artificial intelligence, machine learning, and gene editing, society will undoubtedly find more cures for debilitating disease and succeed in regenerating human health. As science advances, it inevitably intersects with legal and ethical norms, both for individuals and civil society, and there are new externalities to consider. Legal and ethical norms will adapt, rebalancing the interests of each. The fourth industrial revolution is accelerating, and hopefully towards curing disease.